If you have diabetes, you are not alone. Millions of people have it. Many others care about someone who has diabetes.
There is no cure for diabetes yet. But you can do many things to live well with diabetes.
It’s important to learn all you can. The more you know about diabetes, the better you’ll be able to manage it.
If you have diabetes, you are not alone. Millions of people have it. Many others care about someone who has diabetes.
There is no cure for diabetes yet. But you can do many things to live well with diabetes.
It’s important to learn all you can. The more you know about diabetes, the better you’ll be able to manage it.
What is diabetes, and why does it happen?
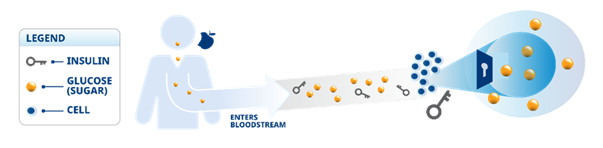
Diabetes is a condition where your body doesn’t make enough insulin, makes no insulin at all, or doesn’t respond to insulin properly. To better understand your diabetes, you need to know what insulin is and why your body needs it.
How eating is related to diabetes
Your cells need sugar for energy. When you eat, some of your food is broken down into glucose (sugar) and enters your bloodstream. Sugar travels in your blood to all of your body’s cells. Insulin is a hormone made by the beta cells in your pancreas. Insulin works like a key to help unlock the cells in your body and lets the sugar in to give you energy. When the sugar moves from the blood into your cells, the amount of sugar in your body goes down.
Understanding diabetes further means knowing the different types of diabetes and their key differences.
Prediabetes
Type 1 diabetes:
Type 2 diabetes:
Diabetes during pregnancy (gestational diabetes):
Diabetes is a condition that changes over time, so it’s a good idea to stay on top of it. No matter what type of diabetes you may have, putting together a diabetes care team can be helpful.
Your team may include:

Be sure to work closely with them. Stay involved, especially with your primary doctor. They’ll help you create a personalized diabetes care plan that can help get you to your goal and keep you there. If you’re not sure where to find each member, ask your primary doctor for help.
Type 1 Diabetes
 The risk factors for type 1 diabetes are still unknown. However, having a family member with type 1 diabetes slightly increases the risk of developing the disease. Environmental factors , consumption of certain food before four months of age (like gluten), exposure to some viral infections , other autoimmune diseases have been linked to the risk of developing type 1 diabetes.
The risk factors for type 1 diabetes are still unknown. However, having a family member with type 1 diabetes slightly increases the risk of developing the disease. Environmental factors , consumption of certain food before four months of age (like gluten), exposure to some viral infections , other autoimmune diseases have been linked to the risk of developing type 1 diabetes.
Genetics
 Having a family history of type 2 diabetes, always puts one at risk of developing type 2 diabetes. Your risk for diabetes is higher if your mother, father or sibling has diabetes. This risk increases as the number of relatives with diabetes increases.
Having a family history of type 2 diabetes, always puts one at risk of developing type 2 diabetes. Your risk for diabetes is higher if your mother, father or sibling has diabetes. This risk increases as the number of relatives with diabetes increases.
Ethnicity
 Diabetes happens more often in Hispanic/Latino Americans, African-Americans, Native Americans, Asian-Americans, Pacific Islanders, and Alaska natives. Studies have shown that being an Asian puts you at a higher risk of developing type 2 diabetes and at younger age when compared with people of European ancestry even at a lower BMI.
Diabetes happens more often in Hispanic/Latino Americans, African-Americans, Native Americans, Asian-Americans, Pacific Islanders, and Alaska natives. Studies have shown that being an Asian puts you at a higher risk of developing type 2 diabetes and at younger age when compared with people of European ancestry even at a lower BMI.
Age
 The risk of type 2 diabetes increases with as one gets older. This may be because one tends to increase weight because of over nutrition, sedentary life style and stress. The risk for type 2 diabetes increases especially after 40 years of age. Although you can't change your age, you can work on other risk factors to reduce your risk. Now a days, type 2 diabetes is also increasing dramatically among children, adolescents and younger adults.
The risk of type 2 diabetes increases with as one gets older. This may be because one tends to increase weight because of over nutrition, sedentary life style and stress. The risk for type 2 diabetes increases especially after 40 years of age. Although you can't change your age, you can work on other risk factors to reduce your risk. Now a days, type 2 diabetes is also increasing dramatically among children, adolescents and younger adults.
Unhealthy Diet
 Unhealthy eating habits, excessive nutrition and a diet rich in sweets and fats leads to overweight which is the most common risk factor of development of type 2 diabetes. A healthy diet is high in fibre and low in fat, cholesterol, salt and sugar. Also it is good to focus on portion size--how much you eat is just as important as what you eat.
Unhealthy eating habits, excessive nutrition and a diet rich in sweets and fats leads to overweight which is the most common risk factor of development of type 2 diabetes. A healthy diet is high in fibre and low in fat, cholesterol, salt and sugar. Also it is good to focus on portion size--how much you eat is just as important as what you eat.
Obesity
 It is one of the top reasons for developing type 2 diabetes. Due to increasing obesity, a growing number of young people are developing diabetes. The more overweight you are, the more resistant your body is to insulin.
It is one of the top reasons for developing type 2 diabetes. Due to increasing obesity, a growing number of young people are developing diabetes. The more overweight you are, the more resistant your body is to insulin.
What is BMI?
Body Mass Index (BMI) is a ratio calculated from weight and height. The BMI is a reliable indicator of body fatness.
Metric BMI formula
BMI* = (Weight in Kilograms / (Height in Meters x Height in Meters)
Physical Inactivity
 The less active you are, ups your risk of developing diabetes. Physical activity helps you control weight, uses up glucose as energy and makes your cells more sensitive to insulin.
The less active you are, ups your risk of developing diabetes. Physical activity helps you control weight, uses up glucose as energy and makes your cells more sensitive to insulin.
Emotional Stress
 For people with diabetes, both physical and emotional stress can take a greater toll on health. In stress, blood sugar levels rise. Stress hormones like epinephrine and cortisol kick in since one of their major functions is to raise blood sugar to help boost energy when it's needed most. More emotional stress worsens the glycaemic control in people with diabetes.
For people with diabetes, both physical and emotional stress can take a greater toll on health. In stress, blood sugar levels rise. Stress hormones like epinephrine and cortisol kick in since one of their major functions is to raise blood sugar to help boost energy when it's needed most. More emotional stress worsens the glycaemic control in people with diabetes.
Know you Number
The first step to diagnosis
If you and your health care provider suspect that you have diabetes, you’ll most likely get a blood test to be sure. There are several types of blood tests that can help your health care provider determine whether you have diabetes. These tests provide a snapshot of your plasma glucose, or blood sugar. These tests include:
Fasting plasma glucose (FPG)
These tests measure a person’s blood sugar after they haven’t eaten for 8 to 10 hours (or overnight). A diagnosis of diabetes is made when 2 fasting plasma glucose tests, taken on different days, are at least 126 mg/dL.
Oral glucose tolerance test (OGTT)
For this lab test, usually taken after an overnight fast, your blood glucose levels are measured before and 2 hours after drinking a liquid that contains glucose (sugar). If your plasma glucose is 200 mg/dL or higher, you may be diagnosed with diabetes.
Random plasma glucose test
With no fasting necessary, this is one of the easiest tests to see if you have diabetes. If you have common symptoms of high blood sugar, such as frequent urination, intense thirst, blurred vision, unexplained weight loss, feeling very tired, and you take a random blood sugar test that shows levels of 200 mg/dL or higher, you may be diagnosed with diabetes.
A1C test
The A1C test measures your estimated average blood sugar levels over the past 2 to 3 months. It’s like a “memory” of your blood sugar levels. An A1C test of 6.5% or higher can be used to diagnose diabetes.
Each diabetes test is different. Some tests tell your health care provider about how your blood sugar levels are doing for a short period of time, like the FPG, OGTT, and random plasma glucose test. Other tests, such as A1C, give your health care team the big picture of what your glucose levels are.
STAYING ON TRACK
A1C vs blood glucose: What are we looking at?
Find out how both blood tests give important insights into your health.
Checking your blood glucose and tracking your numbers is an important part of your diabetes care plan. Both your A1C and your blood glucose levels show how well you’re managing your diabetes. But what’s the difference between these two tests?
Measuring blood glucose
Measuring your blood glucose can show how well your diabetes is controlled from one day to the next. It’s something you can do at home. This test can:

Measuring A1C levels
The A1C test gives the big picture when it comes to your blood glucose. It shows how well you’re controlling your blood glucose over time by measuring the average blood glucose over the past 2 to 3 months. It’s like a “memory” of your blood glucose levels. This is a test you’ll have done at your doctor’s office.
How do A1C levels relate to average blood glucose levels?
When you get your A1C result, you may see a blood glucose reading next to it. This is another way of showing your average blood glucose levels using the same measurement that you see on your meter, mg/dL (milligrams per deciliter).
your doctor will personalize your plan and set goals that are right for you.
How often should you check your blood glucose?
You and your health care professional will decide when and how often you should check your blood glucose. How diabetes affects the body is different for each person and changes over time. So, depending on what medicines you’re taking and your health care professional's directions, your blood glucose testing schedule may change.
You should ask your health care professional when you should call to discuss your blood glucose results. For example, they might say that you should call if your blood glucose levels are lower or higher than usual. Guidelines from the ADA recommend that people contact their doctor if:
Reviewing your blood glucose readings with your diabetes care team can help you find things that can cause your blood glucose to go too high or too low. That way, you can make the changes you need to stay on track!
Remember:
Blood glucose rises right after eating, so check your blood glucose regularly before and after meals to see how certain foods affect your levels.
Okay, I’m taking my medicine. What now?
Have you gotten used to your diabetes treatment? You’re taking your medicine just like your health care professional says? Great, keep up the good work!
But it’s important to remember that there’s more to diabetes management. Now’s the time to think about what else you can do
Build your diabetes care team
You’ve probably already begun this step. But just in case, remember there are a lot of different health care professionals you may want on your team who can help you on your journey. Together, they form part of your diabetes care team.

Eat right
This is a big one. When you eat healthy, you help manage your weight, blood glucose levels, blood pressure—even your mood. Work with your diabetes care team to create a meal plan that’s right for you. Healthy eating is an important part of managing your diabetes along with being active and taking medicines, if needed. Why? Because what, when, and how much you eat affects your blood glucose (blood sugar). It’s also affected by how active you are.
Healthy eating is when you:
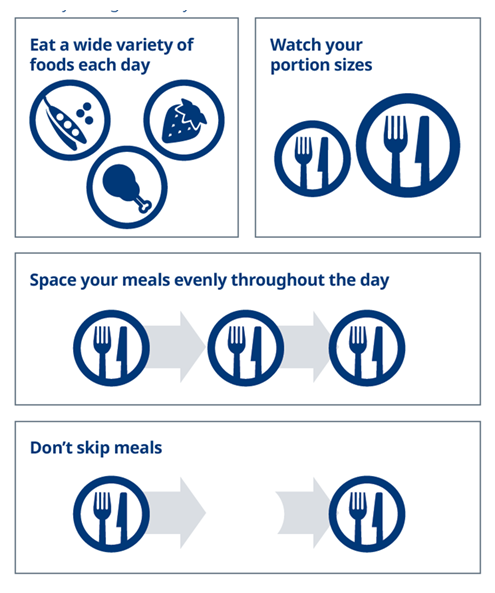
Work with your diabetes care team to find a plan that’s right for you.
Being active
With diabetes, being active and eating healthy work together. Being active may help manage your blood glucose levels. It’s also good for your overall health.
Choosing an activity
Just about anything that gets you moving is good. Choose activities you enjoy, so you don’t give up. You may want to try something new with a friend or family member. You can support and motivate each other to keep going.
Some activities you might want to try:

Always talk with your doctor before starting or changing your physical activity.
Track your blood glucose
Your doctor may want you to track your blood glucose. That’s because it tells you how high or low your blood glucose is, how things like exercise and stress affect it, and how well your medicine is working. You and your diabetes care team will decide when and how often you should check your blood glucose. Talk to your health care professional if tools like a continuous glucose monitor might be right for you.
Reach out for support
Feeling stressed or upset? Your family and friends may be happy to listen and help. Maybe join a support group where you’ll meet other people with diabetes. Chances are they will understand what you’re feeling. They can share ways they manage stress and cope with diabetes. You are not alone!
Let Summarize
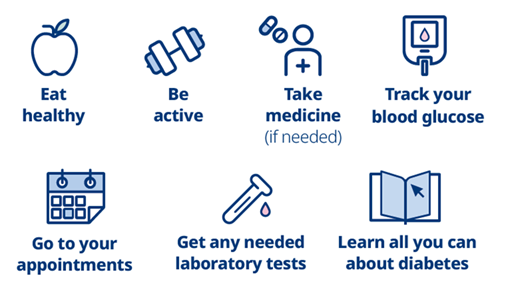
Now is the time to take action to help reduce the risk of long term problems from diabetes.
You probably know that diabetes can be rough on your body. But many signs of the damage diabetes can cause may not show up for several years. Even then, the signs may be so small that you don’t notice them. That’s why it’s important to know what you can do right now to help keep track of and reduce long term problems.
1. Keep things healthy.
Healthy lifestyle habits are important for everyone. And for those living with diabetes, it's especially important to remember these aspects of diabetes care:
2. Take the tests.
The lab tests that your diabetes care team may require can help show if diabetes has caused any health problems.
3. Keep an eye on blood glucose.
This is a big part of diabetes care because over time, high blood glucose (hyperglycemia) can lead to some serious problems. If it’s not controlled, high blood glucose can affect many different parts of the body.
The American Diabetes Association (ADA) has made a list of some common problems. Below, you can find helpful descriptions of each and ways to reduce your risk.
Pay special attention to your feet. Nerve damage and poor circulation can cause problems.
Nerve damage can prevent someone from feeling pain, heat, or cold.
So, if a sore or cut develops, it may not be felt, in which case it might not be treated. As a result, it can get worse and become infected.
Peripheral vascular disease can reduce blood flow to the feet so infections may not heal.
People with diabetes can help protect their feet with these care tips:



The body’s nerves are like wires that send signals to and from your brain.
Over time, high blood glucose can damage the nerves in your body. This damage is called neuropathy.
It is not completely clear why this happens. But people who have had diabetes for a long time are more likely to have some nerve damage.
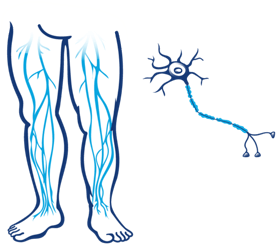
Some of the symptoms of nerve damage may include:
These symptoms may come and go and may feel worse at certain times.
But they can also be caused by other health problems. Be sure to talk with your diabetes care team if you or your loved one with diabetes are having any of them.
Some ways to help reduce the risk of nerve damage are:
High blood glucose can damage the tiny vessels that bring blood to your eyes. This damage can lead to a variety of problems, including loss of vision.

Eye problems, like many other problems of diabetes, don't necessarily have to happen.
Taking these steps may help to protect the eyes:
Your kidneys
The kidneys filter waste products out of the blood. When it is not treated, over time, high blood glucose can damage the small blood vessels in the kidneys. Over time, this may lead to chronic kidney disease (CKD), a progressive, chronic disease that forces the kidneys to overwork and leak useful protein into urine. When kidneys are overworked, it's hard for them to properly filter blood. And after many years, this extra work can cause the kidneys to fail.
Here’s what you can do to care for your kidneys:
Vascular disease can cause damage to the different blood vessels in your body. Oxygen, glucose, nutrients, and other substances travel through our blood vessels to reach the different parts of the body, and a blockage leads to problems.
In peripheral arterial disease (PAD), blocked arteries interrupt blood flow to the legs and can cause these sensations in the legs and feet:
People with diabetes are 2 to 4 times more likely to have vascular disease than people without diabetes. The ADA suggests protecting against vascular disease by following these steps:
One area of the body that people don’t often think about when it comes to diabetes is the mouth.

Diabetes can cause oral health problems. That’s because high blood glucose can add more sugar to saliva, which can help harmful bacteria to grow.
Problems may include:
The dangers of gum disease
Of all the oral problems that can be caused by diabetes, gum disease is perhaps the most dangerous. Why? People with diabetes are more vulnerable to bacterial infections. Once an infection is present, it can be harder to treat in people who have diabetes.
How to protect your teeth and gums:
Other complications
Diabetes is linked to many other diseases and conditions. Many people living with diabetes have at least one other condition. Some common ones include:
Managing your diabetes, including maintaining a healthy A1C and time in range, can help lower your risk of developing complications.
There are many things you can do to manage your blood glucose and live well.
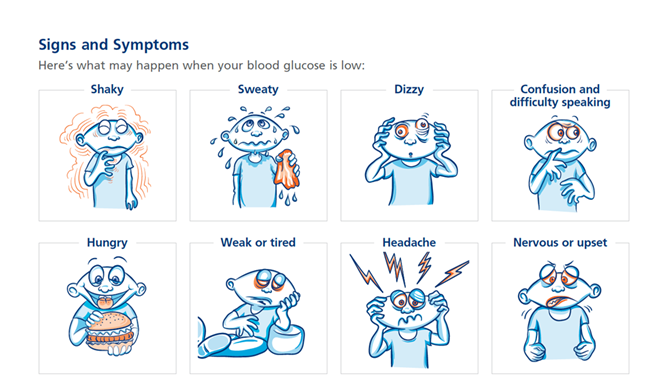
Hypoglycemia is low blood glucose—or low blood sugar—that is below the healthy range. This is usually when your blood glucose is less than 70 mg/dL. You should talk with your diabetes care team about your blood glucose targets, and what level is too low for you.
You may have also heard low blood glucose described as an insulin reaction or insulin shock.
Causes
If low blood glucose is not treated, it can become severe and may cause you to pass out.
If low blood glucose is a problem for you, talk to your doctor or diabetes care team.
Low Blood Glucose (HYPOGLYCEMIA)
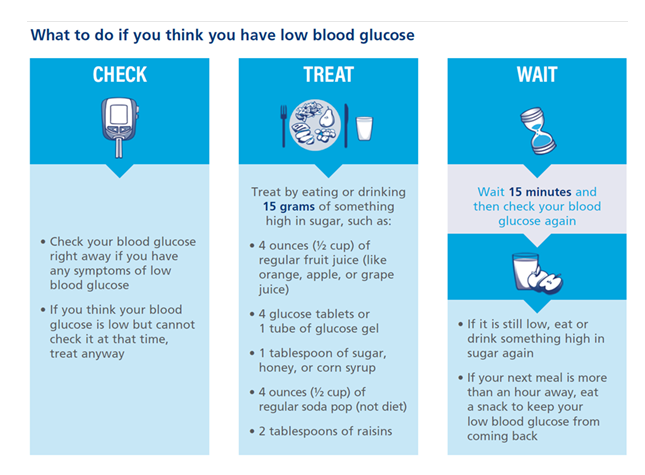
What to do if you think you have low blood glucose
There’s a lot you can do to help keep yourself healthy with diabetes.
High blood glucose (blood sugar) is also called hyperglycemia, which happens when there is too much glucose in your blood. Over time, it can cause serious health problems.
Causes
High blood glucose can also happen as your diabetes changes over time.
Signs and Symptoms
Here’s what may happen when your blood glucose is high:

Or you may have no symptoms at all.
High Blood Glucose (HYPERGLYCEMIA)
What to do about high blood glucose